Public Health England has today released the second tranche of data for COVID tests. This is the most comprehensive data we have for tests as it includes Pillar 1 tests (those conducted by PHE and NHS hospitals) and Pillar 2 tests (those conducted by private companies under NHS Test and Trace).
Some journalists had been using data from coronavirus.data.gov – but this was dangerously misleading as it only revealed Pillar 1 tests – which are now a relatively small proportion of tests. This had led to erroneous league tables based on Pillar 1 data only until the site was updated late on 2 July.
We want to be able to identify possible regions that have the potential to have remedial action taken, for example local ‘lockdowns’, in the future. This does not mean that these areas will be locked down, more that they should be investigated by Directors of Public Health and local journalists. Without specific local knowledge, here are the criteria I have used to identify regions of interest:
HIGH INCIDENCE REGIONS (RED): Greater than 50 cases per 100,000 individuals. While the Joint Biosecurity Centre has not issued public guidelines for this threshold in the UK, Germany has defined 50 cases per 100,000 inhabitants in a week as the number of cases required for a region to apply an ‘emergency brake’ and reimpose restrictions. Areas meeting these criteria could indicate that there is sustained transmission in this area (but see the caveats below).
WATCHLIST REGIONS (AMBER): Between 40 and 50 cases per 100,000 individuals. (The threshold of 40 is chosen based on a qualitative comparison of Barnsley and Bradford in the PHE Leciester epidemiology report.)
RECOVERING REGIONS (GREEN): In a high incidence or watchlist region last week and fewer than 40 cases per 100,000 this week. It is important to bear in mind that no area is recovered from COVID-19, as outbreaks can recur in any region at any time.


A more general point needs to be made about the paucity of publicly available data. Without timely, complete, accurate data available to the public, there are several issues:
- Towns such as Leicester may not understand why they are being locked down, as the maps at the Coronavirus data service do not show anything particularly unusual about Leicester;
- Other towns may see that they have relatively high case levels on the Coronavirus data service, causing unnecessary alarm;
- Having data at a coarse geographical area (currently Upper Tier Local Authorities) does not allow outbreaks in towns and villages to be identified;
- Unitary authorities (such as Leicester – where the city council performs the role of district and county councils) are separated on the maps, but cities such as Oxford (where there is a city council and a separate county council) are included in the data for Oxfordshire, where urban and rural data is evened out, hiding outbreaks in cities.
There are several caveats that need to be emphasized:
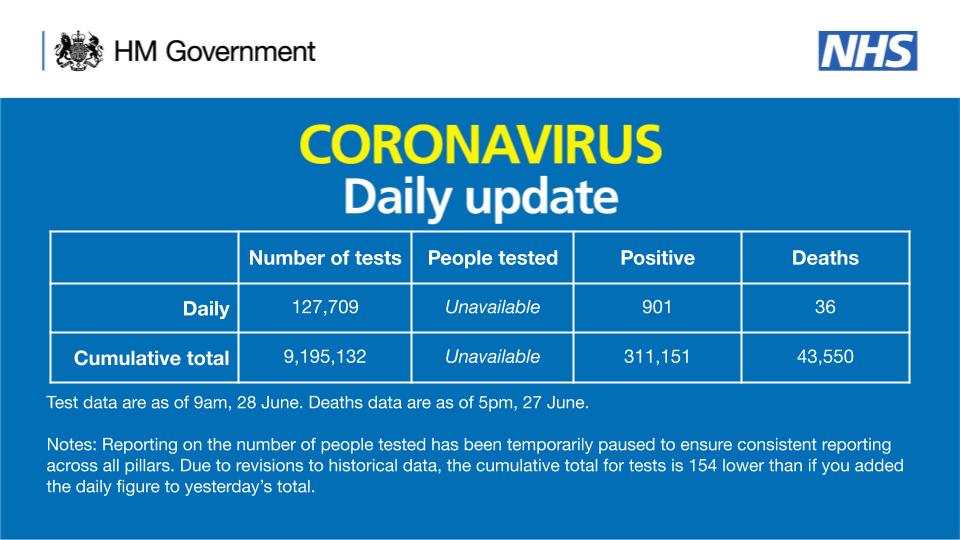
The number of tests carried out: when there are low number of tests, there are necessarily low numbers of detected cases. We do not currently have information for the number of tests carried out in each region, so cannot take account of this – it is possible that high cases per 100,000 is due to particularly high levels of testing in that region.
More local testing in locations with known cases: As local outbreaks are detected, extra testing resources may be allocated to towns such as Leicester, with mobile testing stations being set up. There is a feedback loop here meaning that extra cases will be detected – this does not necessarily mean that there is a higher incidence, just that the cases are being detected.
There is a time lag before this data becomes available: The latest data (published today, 2 July 2020) is for cases detected up to 28 June 2020 – so is not in real-time. In addition, there is a further delay between individuals becoming infected and a case being capable of being detected.
Outbreaks in care homes, hospitals and prisons: These need to be treated independently, and are currently included in the data. We know that there are outbreaks in these locations, and PHE report on these (but we don’t know where these outbreaks are taking place). So Pillar 1 and Pillar 2 data by itself does not indicate that there is community spread – this may be confined to these special locations
Local Directors of Public Health are the experts in their local areas: These professionals are experts, know their communities well, and understand the dynamics of transmission far more than can be ascertained by looking at figures in a database. There have been delays in getting this data to local authorities and issues with data quality, but the Prime Minister has promised in the House of Commons that the data is now getting through.
The delay and lack of detail of Pillar 2 results at district council level, or within-local authority breakdowns (as is disclosed for Pillar 1 tests) highlights data weaknesses, compounding the delays in convening the Joint Biosecurity Centre, and the failure of the centralised NHS Test and Trace App. While directors of public health, Public Health England, NHS Test and Trace, the Joint Biosecurity Centre, and the Department of Health and Social care all play their part, the policy for controlling a pandemic rests with central Government and is ultimately the responsibility of the Prime Minister and the Cabinet. Authority can be delegated but responsibility can not.
For more information, please contact me at d.a.robertson@lboro.ac.uk
or follow me on Twitter @Dr_D_Robertson